KNOW | UNDERSTAND | ACT
How does diabetes relate to cardiovascular disease?
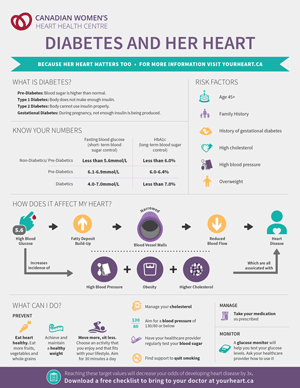 Diabetes or “diabetes mellitus,” is a chronic condition that keeps your body from properly processing the food you eat for use as energy. Generally, the food you eat is turned into sugar, or glucose, that your body needs.
Diabetes or “diabetes mellitus,” is a chronic condition that keeps your body from properly processing the food you eat for use as energy. Generally, the food you eat is turned into sugar, or glucose, that your body needs.
The pancreas, an organ located near your stomach, makes a hormone called insulin, which helps glucose enter your body’s cells and controls the amount of glucose in your blood. Diabetes keeps your body either from producing enough insulin or from using its own insulin as well as it should. This causes sugars to build up in your blood.
When your blood glucose levels are too high, the pancreas releases insulin to stimulate your cells and liver to absorb glucose. This brings your blood glucose levels back to normal.
Hemoglobin A1c (Hb A1c) is a test that provides an average of your blood glucose levels over a prior two- to four-month period. The result indicates how stable your blood glucose levels have been over time.
Blood glucose refers to the amount of sugar in your bloodstream. Glucose is the body’s main source of energy. When blood glucose is high, it is called “hyperglycemia.”
Prolonged high blood glucose levels can increase the buildup of fatty deposits on blood vessel walls, narrowing the walls and reducing blood flow. Over time, these deposits may harden or clog the vessels, resulting in cardiovascular disease. There are three main types of diabetes:
Type 1 Diabetes:
- 5% to 10% of people with diabetes have type 1.
- It usually develops in childhood or adolescence.
- The pancreas is damaged and cannot produce insulin.
- Type 1 diabetes often requires lifelong insulin treatment.
Type 2 Diabetes:
- 90% to 95% of people with diabetes have type 2, the most common form.
- It usually affects adults.
- The pancreas produces too little insulin or can’t use the insulin properly, which results in too much glucose building up in the blood.
- It can be controlled through lifestyle changes and medications.
Gestational Diabetes Mellitus (GDM):
- This type occurs during pregnancy from hormone changes and development of the fetus, which puts added demand on the body to produce sufficient insulin.
- GDM increases the risk for type 2 diabetes later in life; 30% of women with GDM will develop type 2 diabetes within 15 years.
- If appropriate steps are taken for control of blood glucose, a healthy delivery can be expected.
- Being at risk for diabetes doesn’t mean you should avoid getting pregnant.
Pre-Diabetes
“Pre-diabetes” is an important term to become familiar with. It is considered more of a phase of diabetes than a type. If you are diagnosed with pre-diabetes by your doctor, this does not mean you have diabetes.
- Pre-diabetes was once known as “borderline diabetes.”
- It refers to blood glucose levels that are slightly out of range or higher than normal but not enough to be considered diabetes mellitus.
- Pre-diabetes is strongly related to the risk for type 2 diabetes.
- Lifestyle changes prevent or reverse pre-diabetes.
Causes of diabetes
Contrary to popular belief, eating too much sugar does not lead to diabetes. Everyone can benefit from cutting back on sugar, but the cause of diabetes is much more complicated than that: It’s a group of diseases with a range of causes.
Type 1 Diabetes
Type 1 diabetes, the most severe type, is often first diagnosed in children and young adults. It is caused by a faulty immune response in which the immune system attacks part of its own pancreas. The cause is unknown. The immune system treats the insulin-producing cells in the pancreas as invaders, attacking and destroying them, which makes type 1 diabetes an autoimmune disease.
Type 2 Diabetes
Type 2 diabetes, the most common form, tends to occur after age 35, but more and more young people are developing the condition. With type 2 diabetes, the body still produces some of its own insulin, but it’s not enough. Abnormal insulin receptor cells in the body fail to respond to insulin and therefore glucose is unable to enter the cells. This is known as insulin resistance.
What are the symptoms of diabetes?
There may be no signs or symptoms with the onset of type 2 diabetes. However, possible symptoms of diabetes include:
- Unusual thirst
- Frequent urination
- Weight change (unexpected weight gain or loss)
- Extreme fatigue
- Low energy
- Blurry vision
- More frequent infections
- Cuts or bruises that are slow to heal
- Tingling and/or numbness in hands or feet
- Erectile difficulties
Talk with your doctor right away if you are experiencing any symptoms you believe could be associated with diabetes.
Associated risks
Having diabetes can lead to other health problems, especially if your condition is not properly managed or treated. These include the following:
Cardiovascular Disease (CVD) and Stroke
- CVD and stroke occur three to five times more often in people with diabetes.
- 80% of all people with diabetes will die of either CVD or stroke.
- Having diabetes more than triples a woman’s risk of heart attack and greatly increases the chances a heart attack will be fatal. This is because women with diabetes are more likely to experience adverse changes that add to their risk for heart disease. They tend to have greater stores of belly fat and higher cholesterol and blood pressure levels. Also stacking the deck against women is the aging process. They lose estrogen, their natural protection against heart disease, at menopause.
- Type 2 diabetes also leads to a greater risk for cardiovascular complications in women than in men and is a strong risk factor for heart failure. Women account for more than half of the cases of diabetes in the world.
Eye Problems
- Cataracts and glaucoma occur more frequently in people with diabetes.
- Diabetes threatens vision by damaging the retina.
- It is the number one cause of blindness in Canadians.
Kidney Problems
-
Kidney disease is a serious and likely complication in people with long-term diabetes.
Nerve Damage
- Nerve damage is a result of prolonged high blood glucose levels.
- The primary sign of nerve damage is a tingling, numbing, or burning feeling in the hands, feet, arms, or legs. Amputation or loss of a limb may result.
Depression
-
Approximately 25% of people with diabetes will experience depression.
How Is Diabetes Diagnosed?
There are three bloods tests that can help your doctor determine whether you have diabetes:
Fasting Plasma Glucose (FPG): FPG measures the amount of glucose in your blood while you are fasting. Fasting consists of not eating or drinking for at least eight to 10 hours before blood is drawn. Water is acceptable.
Random (non-fasting) Blood Glucose: Blood is drawn at any time of day without fasting.
Oral Glucose Tolerance Test (OGTT): This test allows for two blood samples to be drawn in a two-hour period. The first blood sample is taken immediately after consuming a sweetened drink. You then retake the blood test two hours later to determine whether diabetes is present.
The recommended screening test is the FPG, but a different test may be administered depending on other risk factors and any previous abnormal results.
If your doctor suspects diabetes after giving you the FPG, he or she will likely recommend the oral glucose tolerance test to confirm the diagnosis and determine the appropriate treatment.
How Is Diabetes Treated?
Treatment will vary based on the type of diabetes you have, your risk factors for other conditions, and the test results. Normally, type 2 diabetes can be treated with lifestyle changes and these are important to controlling type 1 diabetes as well. In fact, lifestyle changes alone can reduce your risk of developing type 2 diabetes by as much as 60%. These changes in habits can also help reduce other risk factors, such as high blood pressure and cholesterol. But medications, particularly those targeted to risk factors, may still be necessary.
How Can I Reduce My Risk?
No one knows how to prevent type 1, but paying careful attention to your lifestyle choices can delay or lower your risk of developing all types of diabetes. Healthy eating, regular physical activity and weight control, as well as cholesterol and blood pressure management can all help to slow down or avoid the development of diabetes.
- Eat well by following Canada’s Food Guide.
- Enjoy regular physical activity. Getting at least 150 minutes each week will help keep your blood glucose within a healthy range and promote a healthy weight.
- Achieve a healthy weight. Obesity is a leading cause of type 2 diabetes. Combining physical activity and a healthy diet is the best way to achieve a healthy body weight. In fact, reducing your body weight by 5% to 7% can prevent 58% to 71% cases of diabetes. This video explains how to manage your weight(Ontario Ministry of Health).
Whether you want to prevent diabetes or manage it, having healthy blood glucose levels can greatly improve your overall health and well-being. If you bring your blood glucose within the normal range, you are likely to have more energy, better manage your weight and improve your blood pressure and cholesterol levels.
In fact, effectively managing your blood glucose will help you lower your risk for other health complications, such as cardiovascular disease, stroke, blindness, and kidney disease. If you are already diagnosed and living with diabetes, better glucose management can potentially reduce the amount of medication and/or insulin you require.
Change is possible; hear Susan’s story, along with other real-life stories.
Managing Diabetes
Medication for Type 1 Diabetes
Regardless of your lifestyle, if you are diagnosed with type 1 diabetes, you will require treatment with insulin injections. There are four main types of insulin available. You will be prescribed insulin based on your lifestyle choices, including activity level and eating habits.
The four types of insulin have different activation times following injection:
- Long acting (basal insulin)
- Intermediate acting (basal insulin)
- Short acting (bolus insulin)
- Very rapid acting (bolus insulin)
Each type takes effect at a different rate, peaks at a different time, and varies according to duration. This video presentation offers an overview of insulin (University of Ottawa Heart Institute), its role, side effects, and response time.
The Canadian Diabetes Association provides more information about diabetes products and medications
Medication for Type 2 Diabetes
Type 2 diabetes can be treated with medication to help your body better control blood glucose. Some of the available brand and generic drugs are described in the chart below. Medication is usually started if two to three months of lifestyle management show little or no improvement in blood glucose levels.
This Heart Institute presentation offers an overview of type 2 diabetes medications.
Tips for Managing Diabetes
If you have diabetes, it is important to take your medication and live a heart-healthy lifestyle. The following are tips to help you achieve this:
- Take your medications as prescribed and learn more about managing your medications.
- Learn about managing your diabetes by attending a diabetes education program.
- Monitor and keep track of your blood sugar:
- Target: Blood sugar before meals should be between 4 and 6 mmol/L.
- Target: Blood sugar two hours after meals should be lower than 10 mmol/L.
- Follow the Heart Healthy Nutrition Plan.
- Be active every day. Being physically fit significantly decreases your risk for premature death.
- Achieve and maintain a healthy body weight.
- Ensure good foot health: Take care of your feet.
- Visit your family doctor or diabetes specialist regularly.
It's natural to have questions about what food to eat. A registered dietitian can help personalize your meal plan. If you have diabetes and are taking insulin, speak with your family doctor. You may need to see an endocrinologist (a doctor who specializes in diabetes).
Monitoring Your Blood Glucose Levels
The most important thing about caring for yourself and managing your diabetes is self- testing your glucose levels. You will use a glucose monitor (glucometer) to do this. It will help you keep your levels within a healthy target range.
You can purchase a glucometer at any local pharmacy. Be sure to choose the one that’s right for you. Ask your pharmacist about choosing a glucose monitor. Before you head home with your glucose monitor, be sure you understand how to use it.
This video can help you manage your blood glucose (Ontario Ministry of Health).
How Often Should You Test Your Blood Glucose?
Type 1 Diabetes: At least three times a day with a glucometer. Measure before and after meals
Type 2 Diabetes: At least once a day with a glucometer. Hemoglobin A1c (Hb A1c) is a test that provides an average of your blood glucose levels over a prior two- to four-month period. The result indicates how stable your blood glucose levels have been over time. It should be measured every three months. Talk to your doctor about requesting the blood work.
Gestational Diabetes: Blood glucose should be measured with an oral glucose tolerance test at six weeks and at six months after giving birth. Blood glucose should also be monitored when planning another pregnancy. If diabetes is no longer present after pregnancy, blood glucose should then be monitored every three years (or more often, depending on other risk factors).
Best Practice Guidelines
Download the 2018 Canadian Diabetes Guidelines.

